Navigating the hormonal landscape is a significant part of the transgender journey. Among the various hormones, progesterone often sparks curiosity and discussion within the trans community. What is progesterone? How does it work? What role does it play in the transition process? This comprehensive guide aims to answer these questions and provide an empathetic understanding of progesterone’s place in the transgender journey.
What is Progesterone?
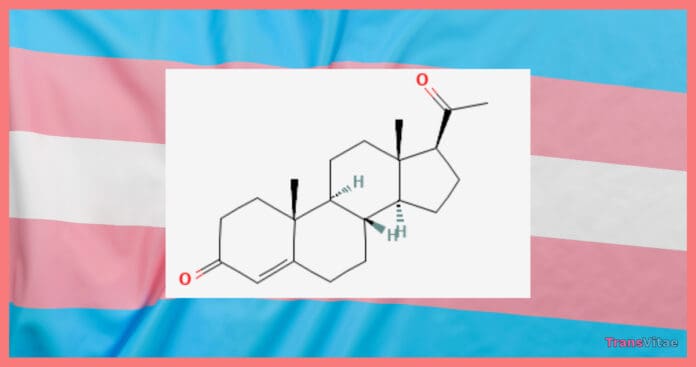
Progesterone is a naturally occurring hormone in the body, predominantly known for its role in the menstrual cycle and pregnancy. In cisgender women, it is produced mainly in the ovaries following ovulation and plays a critical role in regulating the menstrual cycle and supporting pregnancy. However, its functions extend beyond reproduction, influencing a variety of bodily systems, including the nervous system and skin health.
Role in the Menstrual Cycle and Pregnancy
During the menstrual cycle, progesterone levels fluctuate in response to the phases of the cycle. After ovulation, the corpus luteum (a temporary endocrine structure in the ovaries) begins to secrete progesterone. This hormone helps prepare the uterine lining (endometrium) for a potential pregnancy by making it thick and nutrient-rich, creating an optimal environment for a fertilized egg to implant and grow.
If pregnancy occurs, progesterone continues to play a crucial role. It supports the early stages of pregnancy by maintaining the uterine lining and preventing contractions that could dislodge the implanted embryo. Progesterone levels remain high throughout pregnancy, ensuring the developing fetus has a stable environment. The placenta eventually takes over progesterone production to sustain pregnancy.
Beyond Reproduction
While progesterone is essential for reproductive functions, it also affects other bodily systems. In the nervous system, progesterone acts as a neurosteroid, influencing brain function and mood. It interacts with neurotransmitter systems, contributing to mood stabilization and reducing anxiety. Progesterone’s calming effect is particularly noted during the luteal phase of the menstrual cycle, which can help explain some of the mood changes women experience during their cycle.
Progesterone also impacts skin health. It promotes the production of sebum, an oily substance that helps keep the skin hydrated. Additionally, it can enhance skin elasticity and repair, contributing to a more youthful appearance. This effect is beneficial not only for reproductive-aged women but also for post-menopausal women, as maintaining skin health is a common concern with aging.
Impact on the Immune System and Bone Health
Progesterone has a modulating effect on the immune system, helping to maintain a balance between promoting and suppressing immune responses. During pregnancy, this balance is crucial to prevent the maternal immune system from attacking the fetus, which is genetically distinct from the mother. This immunomodulatory effect can have broader implications for autoimmune conditions and overall immune health.
In terms of bone health, progesterone works synergistically with estrogen to promote bone density. It helps regulate bone remodeling by promoting bone formation and reducing bone resorption. This is particularly important for trans women undergoing hormone therapy, as maintaining bone health is a key concern, especially if hormone therapy began later in life.
How Does Progesterone Work?
Progesterone works by binding to specific receptors in the body, influencing gene expression and cellular activity. Its primary functions include preparing the uterine lining for potential pregnancy, maintaining pregnancy, and regulating the menstrual cycle. Additionally, it has a calming effect on the brain, contributing to mood regulation and overall well-being.
Binding to Progesterone Receptors
Progesterone exerts its effects by binding to progesterone receptors, which are present in various tissues throughout the body, including the uterus, breasts, brain, and bones. There are two main types of progesterone receptors: PR-A and PR-B. These receptors are part of the nuclear receptor family, meaning they are located within the cell nucleus and regulate gene expression when activated.
When progesterone binds to its receptors, it triggers a series of molecular events that lead to changes in gene expression. This process involves the receptor-hormone complex binding to specific DNA sequences known as progesterone response elements. By influencing gene expression, progesterone can modulate various cellular functions, such as cell growth, differentiation, and apoptosis (programmed cell death).
Preparing the Uterine Lining
One of the most well-known roles of progesterone is preparing the uterine lining for potential pregnancy. After ovulation, the rise in progesterone levels transforms the endometrium from a proliferative state (where it grows and thickens) to a secretory state. In the secretory phase, the endometrial glands produce nutrients and other factors that support embryo implantation and early pregnancy.
Progesterone also helps maintain the integrity of the uterine lining by preventing its breakdown. If pregnancy does not occur, progesterone levels drop, leading to the shedding of the endometrial lining during menstruation. However, if pregnancy occurs, progesterone levels remain high to sustain the uterine environment.
Mood Regulation and Brain Function
Progesterone’s effects on the brain are multifaceted. It acts as a neurosteroid, meaning it can modulate brain function independently of its role in reproduction. Progesterone influences the activity of neurotransmitters, such as gamma-aminobutyric acid (GABA), which is the primary inhibitory neurotransmitter in the brain. By enhancing GABAergic activity, progesterone can exert a calming effect, reducing anxiety and promoting relaxation.
This calming effect is particularly evident during the luteal phase of the menstrual cycle, when progesterone levels are high. Some women experience a sense of well-being and reduced anxiety during this phase, highlighting progesterone’s impact on mood regulation. Additionally, progesterone has been shown to promote neuroprotection and myelination (the formation of the myelin sheath around nerve fibers), which is essential for proper nervous system function.
Influence on Skin and Hair
Progesterone affects skin and hair health by modulating the activity of sebaceous glands and promoting skin repair. Sebaceous glands produce sebum, an oily substance that helps keep the skin hydrated and protected. Progesterone stimulates sebum production, contributing to skin hydration and overall skin health.
Moreover, progesterone enhances skin elasticity and repair by promoting the production of collagen and elastin, which are structural proteins that maintain skin strength and flexibility. This effect is beneficial for maintaining a youthful appearance and supporting skin health during aging.
In terms of hair health, progesterone can influence hair growth cycles. Some trans women report changes in hair texture and growth patterns when incorporating progesterone into their hormone regimen. While these effects are largely anecdotal, they align with progesterone’s known impacts on skin and hair health in cisgender women.
Immune System Modulation and Bone Health
Progesterone’s impact on the immune system involves modulating immune responses to maintain a balance between promoting and suppressing immunity. During pregnancy, this balance prevents the maternal immune system from attacking the fetus, which is genetically distinct from the mother. This immunomodulatory effect can have broader implications for autoimmune conditions and overall immune health.
Progesterone also plays a role in bone health by working synergistically with estrogen to promote bone density. It helps regulate bone remodeling by promoting bone formation and reducing bone resorption.
Progesterone is a multifaceted hormone with a wide range of effects on the body, extending beyond its well-known role in reproduction. For trans women, understanding progesterone’s functions and how it works can provide valuable insights into its potential benefits and considerations within the context of hormone therapy. Whether it’s contributing to mood regulation, skin health, or bone density, progesterone’s influence is significant and warrants careful consideration and guidance from healthcare providers.
Transgender women undergoing cross-sex hormone treatment experience a range of psychobiological changes over time. This process typically spans an extended period, often two years or more, and involves significant transformations.
Psychological Changes:
- Emotional Shifts: Individuals might notice changes in their emotional responses, often aligning more closely with their gender identity.
- Mental Well-being: Improved mental health has been reported, with reductions in anxiety and depression levels due to increased congruence between gender identity and physical appearance.
Biological Changes:
- Hormonal Dynamics: Hormone levels such as estrogen or testosterone are adjusted to align with the desired gender traits.
- Physical Alterations: These include changes in body fat distribution, muscle mass, and secondary sexual characteristics like voice pitch or facial hair growth.
Overall, these psychobiological changes contribute significantly to the wellness and quality of life of transsexual persons by reinforcing their gender identity on multiple levels.
How Progesterone Interacts with Antiandrogens in Transgender Women
In transgender women, the combination of progesterone and antiandrogens like spironolactone can be pivotal for achieving desired physical changes. Here’s how they work together:
- Regulating Hormone Levels: Progesterone plays a crucial role in managing hormone levels by acting on the hypothalamus. This action helps slow down the release of luteinizing hormone (LH). A decrease in LH results in reduced testosterone production from the gonads. This lower testosterone level is essential for minimizing masculinizing effects and supporting feminization.
- Enhancing Feminization: By contributing to the reduction of testosterone, progesterone aids antiandrogens in shaping a more typically feminine body contour and promoting secondary sexual characteristics. This synergistic effect supports the overall feminization process, complementing the effects of antiandrogens.
- Supporting Antiandrogen Therapy: In the role of a supporting agent, progesterone enhances the effectiveness of treatments like spironolactone. While spironolactone primarily blocks androgen receptors, progesterone’s regulatory influence on hormone balance ensures a more comprehensive approach to hormone therapy.
In summary, progesterone acts in tandem with spironolactone to reduce testosterone levels and boost the feminizing effects of hormone therapy in transgender women.
Progesterone in Transgender Hormone Therapy
In the context of transgender hormone therapy, progesterone’s role is less straightforward but still significant. Trans women may consider adding progesterone to their hormone regimen for various reasons, including potential breast development, mood regulation, and overall feminization. However, the scientific community is still exploring the full extent of its benefits and potential risks for transgender individuals.
Breast Development
One of the most discussed benefits of progesterone in transgender hormone therapy is its potential role in breast development. Some trans women report fuller, rounder breasts when progesterone is added to their regimen. While anecdotal evidence suggests these benefits, scientific studies on this specific aspect are limited. Estrogen is the primary hormone responsible for breast development, but progesterone might play a supplementary role in achieving a more natural breast appearance. However, more research is needed to establish a clear connection between progesterone and enhanced breast development in trans women.
RELATED: Breast Health Essentials for Transgender Individuals
Mood Regulation
Progesterone is known to have a calming effect on the brain, which can be beneficial for mood regulation. For many trans women, transitioning involves a significant emotional journey, and managing mood swings and emotional well-being is crucial. Some studies suggest that progesterone might help stabilize mood and reduce anxiety, although these effects can vary from person to person. Progesterone might help reduce symptoms of anxiety and depression, offering a hopeful perspective on its potential mental health benefits.
Bone Health
Progesterone also plays a role in bone health. Estrogen is known to protect bone density, but progesterone may also contribute by promoting bone formation. For trans women, maintaining bone health is essential, especially if hormone therapy began later in life. While estrogen is critical for bone preservation, progesterone might aid in the maintenance and improvement of bone health, although further research is needed to confirm this effect.
Skin and Hair
Progesterone can influence skin and hair health. Some trans women report improved skin texture and reduced body hair when incorporating progesterone into their hormone regimen. While these effects are largely anecdotal, they align with progesterone’s known impacts on skin health in cisgender women. Progesterone can improve skin hydration and elasticity, providing insights that might be relevant for trans women seeking to enhance their skin health during transition.
Personal Journey with Progesterone
As a transgender woman who started using progesterone nine months into my transition, I can share some personal insights. I initially began with a dose of 100 mg per day and have since increased my dosage to 200 mg per day. While I’ve seen better results, including fuller breast development and improved mood stability, it’s difficult to attribute these improvements solely to the increased dosage. The overall hormone regimen and individual biological responses play significant roles.
RELATED: MTF Transition Timeline: A Guide for Every Step
Understanding Progesterone’s Role in Enhancing Sleep for Transgender Women
When exploring the effects of progesterone on transgender women, one notable area of interest is its impact on sleep. Let’s delve into the benefits progesterone can offer in regulating and improving sleep cycles.
How Progesterone Enhances Sleep
- Natural Sleep Aid: Progesterone is often lauded for its sedative properties, which can aid in calming the mind and promoting a restful night’s sleep.
- Regulation of Sleep Patterns: Research suggests that progesterone helps to stabilize sleep patterns, which is crucial for achieving a healthier and more consistent sleep cycle.
- Reduction of Stress and Anxiety: By potentially reducing levels of anxiety, progesterone indirectly contributes to a more relaxed state, making it easier to fall asleep and stay asleep.
Improved sleep is essential not only for daily function but also for overall health. A balanced sleep cycle supports mental well-being, boosts mood, and enhances cognitive functions—all vital components during the transition process for transgender women.
Incorporating progesterone into a regimen can provide beneficial effects on the sleep cycle, supporting better rest and recovery. Understanding these benefits can empower transgender women in making informed decisions about their health and transition journey.
How Can Progesterone Help with Estrogen Withdrawal Symptoms in Transgender Women?
Transgender women undergoing estrogen therapy often face the need to pause treatment before gender affirmation surgery. This pause can lead to uncomfortable withdrawal symptoms, with hot flashes being a common issue.
The Role of Progesterone
Progesterone can play a crucial role in alleviating these symptoms during the withdrawal period. Here’s how:
- Symptom Relief: Progesterone is known to help reduce symptoms such as hot flashes, which are often experienced when estrogen levels drop.
- Hormonal Balance: Although originally part of the menstrual cycle, progesterone can assist in balancing hormone levels when estrogen is unavailable, providing a smoother transition and lessening the intensity of withdrawal effects.
- Mood Stabilization: By acting on the central nervous system, progesterone may contribute to mood stabilization, which is particularly beneficial when hormonal changes can lead to emotional fluctuations.
- Bone Health Support: Progesterone may also offer additional benefits, such as supporting bone health, which is important when estrogen, a key player in maintaining bone density, is temporarily withdrawn.
By incorporating progesterone treatment during this critical time, transgender women can find relief and maintain a sense of stability until they can resume estrogen therapy post-surgery.
Risks and Considerations
While progesterone offers potential benefits, it’s crucial to consider the risks and side effects. Progesterone therapy can cause mood changes, weight gain, and an increased risk of blood clots, particularly when combined with estrogen. Monitoring and managing these risks with the help of a healthcare provider is essential.
Mood Changes
Progesterone can affect the brain’s neurochemistry, leading to mood swings, irritability, or even depression in some individuals. It’s essential to monitor these changes and discuss them with a healthcare provider, who can adjust the hormone regimen or provide additional support if necessary. Some individuals may find their mood stabilizes with progesterone, while others may experience increased anxiety or depressive symptoms.
Weight Gain
Weight gain is another potential side effect of progesterone therapy. This can be due to increased appetite, water retention, or changes in fat distribution. While some weight gain might be minimal and manageable, significant changes should be discussed with a healthcare provider. Adopting a balanced diet and regular exercise routine can help mitigate some of these effects.
Increased Risk of Blood Clots
One of the more serious risks associated with progesterone, especially when combined with estrogen, is an increased risk of blood clots. Blood clots can lead to deep vein thrombosis (DVT), pulmonary embolism, stroke, or heart attack. It’s crucial for individuals on hormone therapy to be aware of the symptoms of blood clots, such as swelling, pain, redness in the legs, or sudden chest pain and shortness of breath. Regular medical check-ups and discussions with a healthcare provider are vital to managing this risk.
Liver Function
Oral progesterone, in particular, can affect liver function due to its first-pass metabolism through the liver. This implies that the hormone goes through the liver’s processing process before entering the bloodstream, which may result in increased liver enzyme levels and potential liver strain. Regular liver function tests are recommended to ensure that the liver is handling the hormone therapy well.
RELATED: The Benefits of Milk Thistle in Combination with Oral Hormone Replacement Therapy (HRT)
Individualized Hormone Therapy
Each person’s response to hormone therapy is unique, necessitating an individualized approach. What works for one individual may not work for another, and dosages or forms of progesterone might need adjustment over time. Healthcare providers specializing in transgender health can tailor hormone regimens to meet individual needs, minimizing risks while maximizing benefits. Open communication with healthcare providers about any side effects or concerns is critical to successful hormone therapy.
RELATED: Your Transgender Journey: A Guide to Self-Discovery, Transition, and Thriving
Choosing the Right Form of Progesterone
Progesterone is available in various forms, including oral pills, creams, and injections. Each form has its pros and cons, and the choice depends on individual preferences, medical history, and the advice of a healthcare provider.
Oral Progesterone
Oral progesterone is the most common form of progesterone used in hormone therapy. It is convenient to take, as it comes in pill form and can be easily incorporated into a daily routine. However, oral progesterone can cause gastrointestinal side effects such as nausea and bloating. Additionally, it has a higher risk of affecting liver function, so regular monitoring of liver enzymes is essential for those taking oral progesterone. Despite these potential drawbacks, oral progesterone remains a popular choice due to its ease of use and widespread availability.
Topical Progesterone
Topical progesterone creams are applied directly to the skin and are often used for their localized effects. These creams can be applied to areas such as the inner arms, thighs, or abdomen. One of the main advantages of topical progesterone is that it bypasses the gastrointestinal system, potentially reducing the risk of gastrointestinal side effects. However, the absorption rate can vary significantly between individuals, making it challenging to achieve consistent hormone levels. The effectiveness of topical progesterone can also depend on the specific formulation and the area of application. Regular blood tests are recommended to ensure adequate absorption and hormone levels.
Injectable Progesterone
Injectable progesterone provides a more controlled delivery method, ensuring a consistent dose of the hormone is absorbed into the body. It is administered through intramuscular injections, typically every one to two weeks. This form of progesterone can be particularly beneficial for those who have difficulty absorbing oral or topical forms. However, the injections can be painful and inconvenient, requiring regular visits to a healthcare provider or self-administration if properly trained. Additionally, careful dosing and monitoring are necessary to avoid potential side effects and ensure optimal hormone levels.
Rectal Progesterone (Boofing)
Some trans women choose to administer their progesterone dose rectally, a process colloquially referred to as “boofing.” This method involves inserting progesterone suppositories or capsules into the rectum, where the hormone is absorbed through the rectal mucosa. Boofing can improve absorption and reduce gastrointestinal side effects compared to oral progesterone. However, it should only be done under medical supervision to ensure proper dosing and avoid complications. Rectal administration may also be less convenient and more uncomfortable for some individuals.
Personal Stories and Testimonials
Hearing from other trans women about their experiences with progesterone can be incredibly valuable. Many trans women have shared their stories online, providing insights into the benefits and challenges they have faced with progesterone therapy.
For instance, a good friend of mine, a trans woman who started progesterone therapy two years into her transition, reports that it significantly improved her breast development and mood stability. She highlights the importance of working closely with her endocrinologist to find the right dosage and form of progesterone that worked for her.
The Bottom Line
Progesterone is a complex but potentially beneficial hormone in the transgender journey. While research is still evolving, many trans women find that adding progesterone to their hormone therapy can enhance breast development, improve mood, and offer other feminizing effects. However, it’s essential to approach progesterone therapy with caution, under the guidance of a knowledgeable healthcare provider, and with an understanding of the potential risks and benefits.
Trans women, their families, and allies should be well-informed about progesterone to make empowered decisions that best support their transition goals and overall well-being. As with all aspects of hormone therapy, individual experiences with progesterone can vary, so personalized care and open communication with healthcare providers are key.
Progesterone’s role in transgender hormone therapy is an ongoing area of research, and staying informed about the latest studies and medical advice is crucial. By understanding progesterone and its potential impacts, trans women can better navigate their hormonal journey and achieve their transition goals with confidence and care.
For further information and support, consider consulting with a healthcare provider who specializes in transgender health, joining support groups, and accessing resources from reputable transgender health organizations. The journey of understanding and utilizing progesterone is unique for each individual, and with the right support and information, it can be a fulfilling part of the transgender experience.